Welcome to Part 2 in my series on Pregnancy with A Spinal Cord Injury.
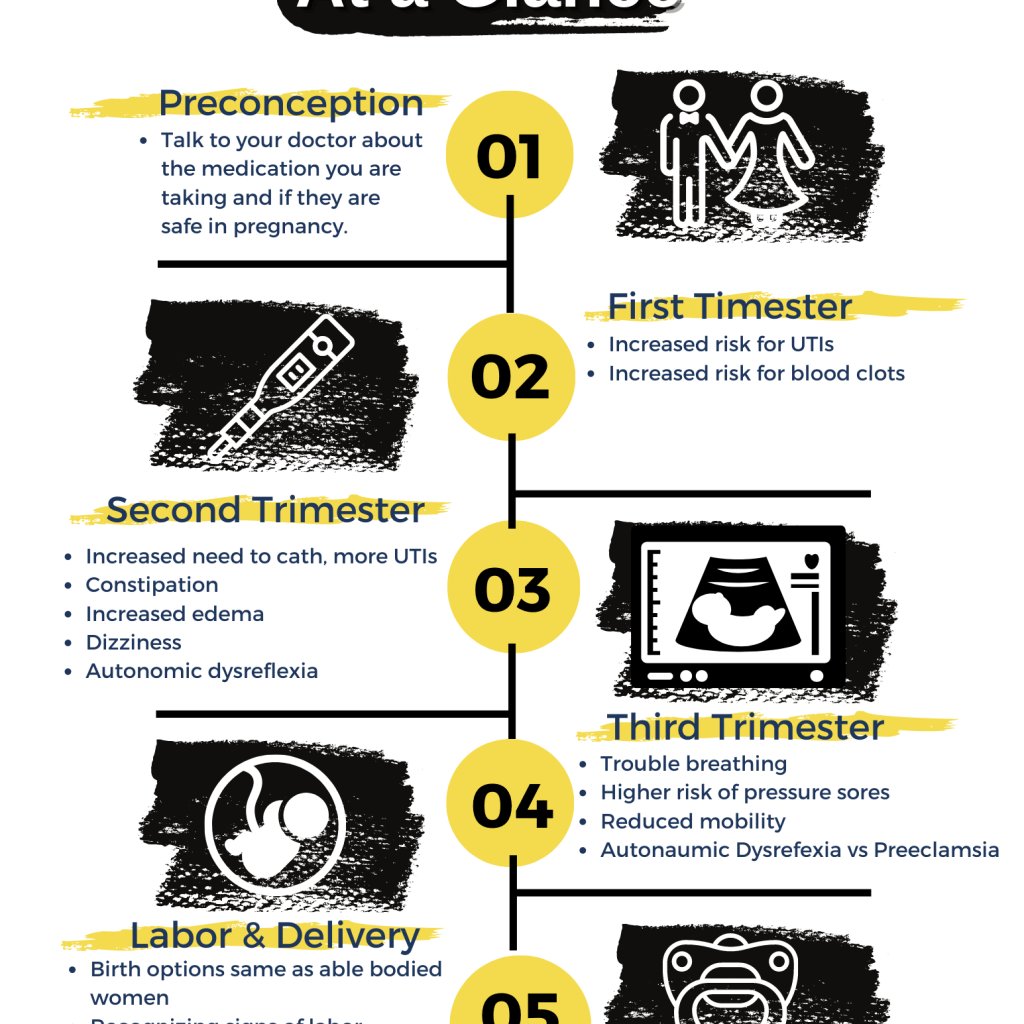
In Part 1, we talked about medication use during pregnancy, UTI risks and how to treat UTIs during pregnancy, as well as blood clot risks associated with pregnancy and preventative steps that you might be advised to take.
Part 2 is all about the second trimester. By now the baby will be growing, your body will be going through some more noticeable changes and the pregnancy will start to influence many of the everyday issues that you face with a spinal cord injury.
With the right planning and lifestyle modifications, the changes that the second trimester brings can be managed comfortably.
So without further adieu, here are the important things that you need to think about and discuss with your doctor in the second trimester of pregnancy.
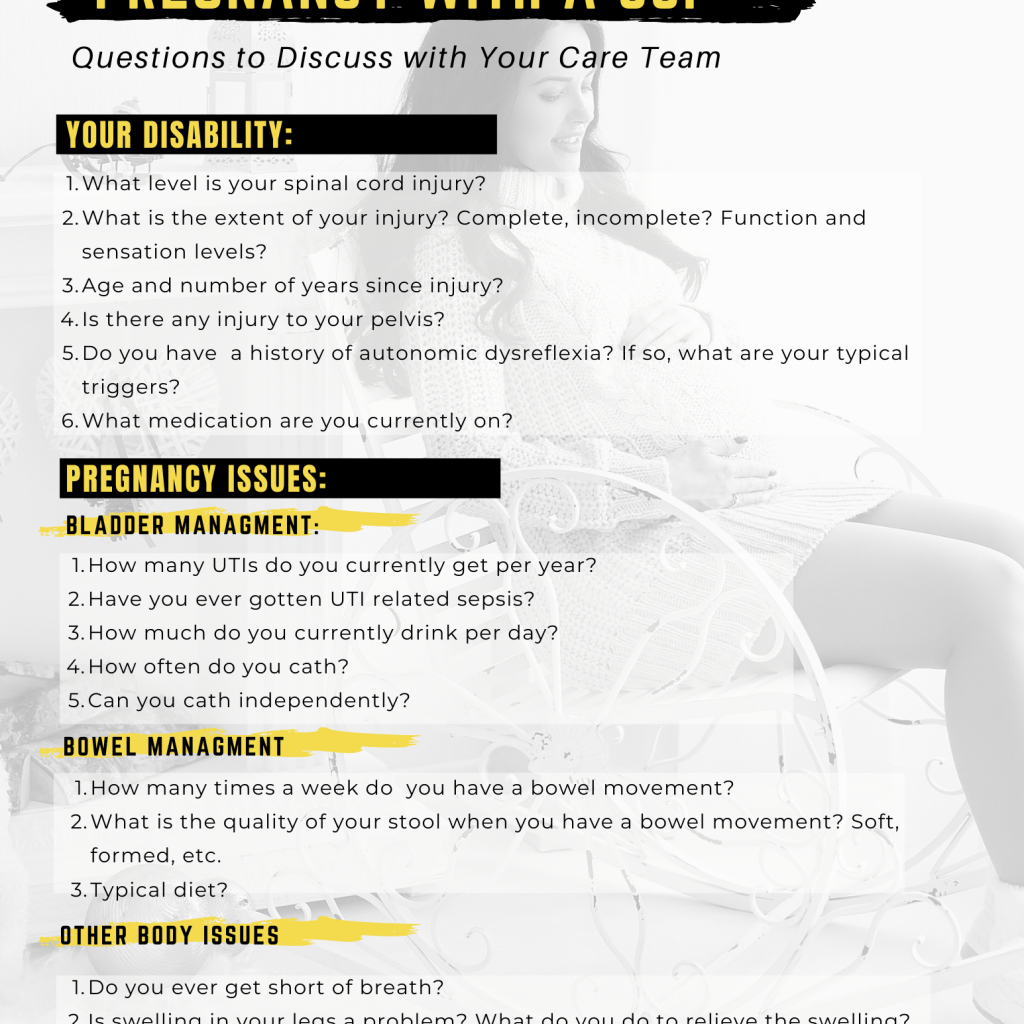
Bladder Management
Bladder management becomes more of a concern in the second trimester. The growing baby puts increased pressure on the bladder. Drinking more to prevent UTI’s and an increased blood volume that occurs during pregnancy mean that urine output is higher. The combination of these issues can make bladder spasms worse and require you to catheterize more frequently. It can also cause more incontinence. Some women may require a foley catheter near the end of the pregnancy if the incontinence becomes too bothersome. UTIs continue to be a major concern in the second trimester as they can cause preterm labor. Making sure you are taking steps to prevent UTIs and having your doctor follow you closely to monitor for symptoms of a UTI is critical. It may be necessary to take a prophylactic antibiotic if UTIs become too frequent.
My Personal Experience
I had recurrent UTIs throughout both of my pregnancies and with the UTIs came incontinence. However, I had recurrent UTIs before my pregnancies so this wasn’t much of a change for me. I wasn’t any more incontinent while I was pregnant than I normally was. I did find that I had to cath more often which was slightly inconvenient because I was washing catheters at the time. The more frequently I peed the more catheters I had to think about washing and drying. I had to have about a 10 day rotation going so that I had enough dry catheters to use. If I could go back and do it all over again I would DRINK WAY MORE. I just didn’t really know better at the time. You live you learn!
As mentioned in Part 1 of the series, my recurrent UTIs caused me to go into labor early with my daughter so MAKE SURE YOU ARE TAKING PREVENTATIVE MEASURES!
Bowel Management
The pregnancy hormone progesterone relaxes smooth muscles in the body, including your intestines. This reduced tone in your digestive tract slows digestion and can cause constipation. Individuals with spinal cord injuries are already at higher risk for constipation due to a reduction in bowel motility and an increase in bowel transit time and pregnancy tends to exacerbate the situation. It may be necessary to eat more insoluble fiber (broccoli, kale, spinach, brussel sprouts, whole grain products, etc) during pregnancy and take natural (senna tea, prunes) or pharmaceutical (bisacodyl, MiraLax) medications to maintain regularity.
My Personal Experience
To be honest I don’t remember whether my bowels changed much in my pregnancies (after all my son is 12 now!!). I did struggle with constipation on a regular basis so I am assuming that it stayed about the same or I would have remembered I think. I didn’t eat very healthy at the time so that probably didn’t help. I have since completely change my diet and only have the occasional problem with constipation. My favorite ways to help stay regular are drinking ginger tea, taking magnesium, and eating lots of veggies!
Faintness and Dizziness
The pregnancy hormones that are responsible for relaxing the smooth muscles of the digestive tract also relax the walls of veins. This, coupled with the increased pressure that the uterus puts on veins, means that the blood returns to the heart more slowly. Blood pressure can decrease and cause dizziness and/or an increased heartbeat.
My Personal Experience
Dizziness was a huge problem for me in my first pregnancy. I didn’t understand the science behind by lightheadedness at the time though. I just knew that I had to lie down A LOT. I remember lying down multiple times a day sometimes. In my second pregnancy this was not as much of a problem probably because I had a 4 year old that I needed to take care of and I couldn’t just lay down whenever I felt like it.
Edema
A number of issues increase the chances for edema during pregnancy. An increase in blood volume means an increase in fluid circulating throughout the body and more relaxed veins due to hormones means fluid has more time to escape from the blood into the interstitial spaces in between the cells in the body. This is usually mildly bothersome and can be treated with compression stockings or more frequently elevating your feet.
My Personal Experience
I didn’t notice any extra swelling in either of my pregnancies. I often laid down in my first pregnancy which probably helped keep the swelling down and in my second pregnancy I was wearing shoes most of the time which usually stops my feet from swelling too much.
Autonomic Dysreflexia
There are many SCI related issues that can become more problematic during pregnancy and trigger autonomic dysreflexia. Increases in bladder spasms, more frequent UTIs, constipation, increased edema and weight gain can all cause uncomfortable stimuli that may cause dysreflexia. Monitoring your blood pressure regularly, managing your symptoms, and taking care to prevent or remove the uncomfortable stimuli are important steps to take to mitigate the risks.
My Personal Experience
This was a really big concern of mine in my first pregnancy. I was really paranoid about getting autonomic dysreflexia and checked my blood pressure constantly. Luckily I didn’t have true dysreflexia often throughout the pregnancy. I did, however, have anxiety often which raised my blood pressure and worried me about the possibility of dysreflexia. If you are prone to anxiety like I am, I suggest talking to your doctor about the difference between anxiety related blood pressure spikes and true autonomic dysreflexia. It took me many years to be comfortable knowing the difference between the two because the symptoms can be very similar sometimes.
Summary
- Bladder management changes as the baby puts more pressure on the bladder and fluid volume increases.
- Progesterone relaxes the intestines often causing constipation. You may have to change your diet during pregnancy or take laxatives to stay regular.
- Blood circulates more slowly during pregnancy, which can make blood pressure drop and cause dizziness.
- Swelling in your feet and legs may increase due to slower circulation and increased pressure on veins in the lower body.
Getting into a Routine
The second trimester is all about adjusting to the major body changes that occur and getting into a new routine with your bowel, bladder, and activity levels if needed. These months can feel really stressful but if you make the changes early and find a rhythm, them the third trimester can be a time to relax and get ready for the baby! Listen to your body and give it what it needs!
Good luck!
For more information check out the last post in the series:
And if you didn’t get a change to download your free pregnancy resources yet you can grab them here:
Pregnancy with a Spinal Cord Injury at a Glance
Questions to Discuss with your Care Team Before and During Pregnancy