This is a 3 Part Series on Pregnancy with a Spinal Cord Injury. When I got pregnant in 2008, there was exactly zero information on the internet about pregnancy with a disability. I had NO IDEA what to expect and had no one to turn to that could answer my questions.
My gynecologist and I fumbled thorough my pregnancies with the limited information that we both knew, and leaned on my Physiatrist to fill in the gaps. In an attempt to get some advice from people that were actually in the same situation as me, I contacted my local rehab hospital and asked if they knew anyone with a spinal cord injury that had had kids post injury. They gave me a few names and I met with a few families.
Let’s just say the families I met with weren’t exactly inspirational. One had a full time nanny (which is totally ok if that’s what you want) and another mom made due with some questionable parenting techniques because she didn’t have any accessible equipment. These situations only made me more nervous about being a mom.
Luckily (although at the time I though he was being a total jerk) my husband refused to get a nanny and gave me a good talking to about how capable I was. I got off to a rough start when my son was first born but pretty soon I figured out how to be a mom, wheelchair and all.
And so can you.
But first the pregnancy…..
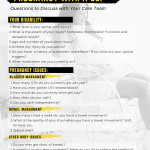
Here are the most important things I think you should know and be ready to discuss with your doctor at your very first appointment.
Medication
Most woman with spinal cord injuries are on some kind of medication for spasticity, bladder control, pain, or all of the above. Not all of these medications are safe during pregnancy, so ideally any pregnancies should be planned and you should talk to your doctor preconception about the medications you’re taking and which ones are safe. If you are taking medication that is unsafe, then you and your doctor can decide whether to stop taking the medication or find alternatives that are safe to take throughout the pregnancy and for breastfeeding.
My Personal Experience
I got pregnant in my second year of university, just 6 months after I started dated my now husband. I was so ready to be a mom and was super exited when I found out. Um….. it was unplanned and I was terrified. It took me about 3 months to get up the nerve to tell my parents. I was 21 and for some reason I still felt like I was gonna get in trouble. I hadn’t really figured life out as an adult yet, let alone one in a wheelchair, and now I had to think about being pregnant, and then a mom, and still somehow finishing university.
Long story short, because the pregnancy was unplanned, I didn’t think about the medications I was on before conception. At the time I was taking 40 mg of baclofen 4x/day (so 120 mg/day) and 5 mg of oxybutynin 4x/day (so 20 mg/ day). My doctors and I decided that it was probably better for both the baby and I that I stay at my current dose of both medications since the withdrawal process from such a high dose of baclofen would take almost the entire pregnancy (weaning off of baclofen must be a very slow and controlled process to avoid neurological dangers such as seizures) and that I would need my bladder control medication to stay comfortable throughout my pregnancy.
When I got pregnant the second time, I opted to stay on the same dosages.
Did the drugs have any effects on my babies?
Yes and no.
Both of my babies went through baclofen withdrawal. I didn’t really know the signs of baclofen withdrawal when my son was born and because I was discharged from the hospital relatively quickly none of the doctors that saw my son after he was born noticed the baclofen withdrawal either. I remember him being very twitchy as a newborn. At the time I thought that he was just easily startled by noises and didn’t think much of it. The twitching took about 2 weeks to subside and then there were no noticeable side effects from the baclofen that I can recall.
When my daughter was born, I went into labor early. She was born 5 weeks premature and had to stay in the NICU. While she was there, the doctors noticed her withdrawal symptoms. It was only when they pointed them out to me that I realized that the twitching my son had experienced was part of the baclofen withdrawal too. They supplemented my daughter with very low doses of baclofen and weaned her off slowly so that the withdrawal would be more comfortable for her.

In hindsight, I wish I would have lowered my dosages of baclofen for my second pregnancy. I have since cut my baclofen usage in half in an effort to reduce the amount of medication I am taking. I am not sure whether it would have reduced the withdrawal symptoms that my kids expereinced but I think I would have liked to try just in case.
Apart from the baclofen withdrawal, there were no noticeable side effects from the medications when they were born.
Both of my kids have developed transient tick disorder as they have gotten older, which is similar to Tourette’s syndrome except with no psychological difficulties. The ticks are not very mild and range from throat clearing to frequent stomping when my daughter walks. Even though this isn’t a documented long-term effect of baclofen use during pregnancy, I often wonder if there is a connection. This is purely speculation but something I thought I should mention.
Below is a summary of some of the common drugs used by women with spinal cord injuries and their safety in pregnancy.
Disclaimer: This information is for educational purposes only and is not intended to recommend, diagnose, or suggest a course of action. ALWAYS talk to your doctor before starting or stopping any drugs.
[table id=2 /]
Blood Clot Risk
Blood volume increased significantly during pregnancy making the risk for blood clots higher for all pregnant woman. Spinal cord injury is already a risk factor for developing blood clots so adding pregnancy increases the overall risk. You and your doctor can discuss your individual health history and lifestyle and decide if preventative steps should be taken. Often compression stockings and regular range of motion exercises are the only recommendations. More aggressive preventative measures such as Venapro DVT Compression Therapy may be necessary if it is determined that your risk is significant.
My Personal Experience
In neither of my pregnancies did my doctors recommend a specific course of action to prevent blood clots. Being fairly active and with a healthy amount of spasticity, my doctors decided that my risk for blood clots was likely not much higher than an able bodied woman. I had C-sections for the birth of both children and after my surgeries I do remember getting a single shot of a blood thinner as a precaution because surgery also increases the risk for blood clots.
Urinary Tract Infections
Pregnancy increase the risk for UTIs in all women and can be especially common for women with SCI. This complication can not be stressed enough. UTIs left untreated can lead to sepsis and are a risk factor for preterm labor. It is important to discuss possible treatment options if you are prone to chronic infections. It may be advised that urine cultures be taken frequently to check for UTIs or that antibiotics be taken throughout the pregnancy to prevent UTIs altogether.
My Personal Experience
I had chronic UTIs for the first 15 years after my spinal cord injury, including throughout both of my pregnancies. In my second pregnancy they were much worse than in my first. My doctor was treating them each time, but they just kept coming back. Near the very end of my second pregnancy, I happened to see a different doctor, that was filling in for mine when she was on holidays, who finally did what should have been done much earlier in the pregnancy; put me on a low dose antibiotic to prevent further UTIs. I went into labor shortly after starting the antibiotics and I believe that the chronic UTIs were the reason. I think the proper treatment was just started too late.
Summary
- Not all spinal cord injury related medications are safe during pregnancy. It is important to have a conversations with your doctor about your medication needs. Ideally this conversation should happen before becoming pregnant, but if not then at the very first appointment!
- Blood clot risk increases during pregnancy due to increased blood volume. Your lifestyle and medical history will determine whether there is a need for preventative measures.
- UTIs can be a serious problem for pregnant woman with spinal cord injuries. They are a risk factor for preterm labor and can lead to sepsis. Prevention is important whether it be through lifestyle modifications or antibiotics.
Be Prepared
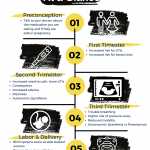
Finding out you are pregnant is exciting. But it can also be really scary. Especially when you have a spinal cord injury. It is important to be prepared for the unique challenges that having a spinal cord injury can bring during pregnancy and make a plan for handling them if they should arise.
You got this! Best of luck with your pregnancy!
Here are a few gifts for you to help make your pregnancy easier:
Pregnancy with a Spinal Cord Injury: At A Glance
Questions to Discuss with Your Doctor Before and During Pregnancy