Welcome back to the third and final blog in my series on Pregnancy with a Spinal Cord Injury.
In Part 1 we talked about medication, UTIs, and blood clots. In Part 2 we talked about bladder, bowel, dizziness, swelling, and autonomic dysreflexia.
This final part in the series is all about the changes that happen to our body as we near the end of our pregnancy and making a birth plan that we can be comfortable with.
Let’s dive right into all the things you need to know in the third trimester!
Breathing Issues
As the fetus grows, the uterus begins to displace organs, including the diaphragm, the main respiratory muscle. When this happens lung capacity decreases and breathing may become more difficult. Women with higher level spinal cord injuries may need supplemental oxygen near the end of the third trimester if oxygen levels dip too much.
My Personal Experience
I was really lucky and didn’t experience any breathing issues with my pregnancies. I have to admit, I wasn’t very active near the end of my pregnancies so I didn’t challenge my breathing at all. If I had I may have noticed a difference in my lung capacity.
Skin Issues
Weight gain, nutrient deficiencies, anemia, and changes in center of balance can make skin more vulnerable to breakdown during pregnancy. Remembering to eat a diet with adequate protein and with important nutrients like zinc, vitamin A, and vitamin C will be important throughout the pregnancy to maintain tissue integrity. It is also important to stay hydrated to improve elasticity and prevent dryness. This will help prevent pressure sores as well as reduce the risk for stretch marks. Pressure relief should be a priority. The last thing that you need is to get a major pressure sore right before the birth of your baby!
My Personal Experience
I did not get a pressure sore in either of my pregnancies, nor did I seem to have any noticeable skin issues. HOWEVER, I did get a pressure sore when my son was just 6 months old because I wasn’t paying enough attention to pressure relief after he was born. This was a giant inconvenience. My sister had to come and stay with me for a few weeks to help take care of my son so that I could stay out of my wheelchair. I also had to go and stay with my mom for a few weeks to get help. If I hadn’t had people that I could turn to I am not sure what I would have done. Making it a priority to do pressure lifts throughout the day is WAY easier than having to stay out of your wheelchair for hours at a time. So do whatever you have to do to remember to do lifts. Set an alarm on your phone, post signs around the house. Whatever. Just do it.
Mobility
Weight gain and a growing belly will make everyday tasks more difficult and awkward. Care should be taken when transferring. Additional support and equipment may be necessary for safety. Using a transfer board or waiting until someone else is home before transferring to a shower or toilet are just a few of the precautions that could be considered in as you move into the third trimester.
My Personal Experience
There was never a time during my pregnancies that I wasn’t able to transfer myself but I made sure that I didn’t do bowel routine our shower unless my husband was home.
Preeclampsia OR Autonomic Dysreflexia
Preeclampsia more commonly occurs in the third trimester. The symptoms of preeclampsia closely mimic those of autonomic dysreflexia so it is important that your doctor is knowledgeable about AD and can properly distinguish one from the other. The symptoms of both of these conditions are very similar but the treatment is very different. It is also important never to assume that your symptoms are AD. If you are experiencing high blood pressure it is important to get it checked out.
This is especially important near the end of the pregnancy when labor is near. One indication that high blood pressure is caused by dysreflexia and not preeclampsia is if the blood pressure spikes occur with contractions. If blood pressure goes down in between contractions it likely autonomic dysreflexia and not preeclampsia.
ALWAYS get symptoms checked in the third trimester.
What is preeclampsia?
Preeclampsia is hypertension during pregnancy, thought to be caused by genetic factors, autoimmune disorders, and blood vessel abnormalities. It can lead to eclampsia, a life threatening condition.
My Personal Experience
I got autonomic dysreflexia more often in the third trimester of both of my pregnancies. It was mostly a problem with Braxton Hicks contractions. None of my doctors ever warned me about preeclampsia but they did tell me to watch for tell-tale signs of dysreflexia with contractions.
Labor and Delivery
Birth Options:
A vaginal birth is the preferred option for women, including those with spinal cord injuries. Cesarean sections are normally considered for medical reasons. It is important that no doctor insist on a C-section for their own comfort. Vaginal births are safe and effective regardless of level of injury.
My Personal Experience
I had no idea that a vaginal birth was an option when I first became pregnant. I assumed that because I couldn’t push, a C-section would be the only option for women with spinal cord injuries. It wasn’t until my doctor told me an interesting fact that I realized vaginal births are just as effective for woman with SCI. She told me that often abled bodied women fight the birthing process because they are in so much pain (and therefore their muscles are tense) and that paralyzed women often have faster births because their natural contractions are able to have more effect in the absence of pain. Even though I learned this, I opted for C-sections because my mom was never able to dilate properly and I didn’t want to take the chance of any complications during the birth of my children. In hindsight, I wish I would have tried a vaginal birth. My doctors definitely didn’t encourage me to do a vaginal birth so I think that was partly why it was such a quick decision to go with a C-section.
Recognizing Signs of Labor
Most women with spinal cord injuries won’t be able to feel the pain of contractions so being able to identify other signs of labor is important. Other signs of labor include general discomfort, back and shoulder pain, sinus pain, bladder spasms, increased spasticity, and autonomic dysreflexia. Sometimes a doctor will choose to induce early to lessen the chances that a woman with a spinal cord injury will go into labor without knowing. Some doctors may even choose to use a contraction monitor along with regular monitoring of cervical dilation. (1) (2)
My Personal Experience
With my first pregnancy the doctor scheduled my C-section a few weeks in advance of my due date to reduce the chances that I would go into labor without knowing. I didn’t have any major contractions before the scheduled C-section. With my second pregnancy I went into labor 5 weeks early. I could not feel the pain of the contractions but I could feel the pressure and tightness in my abdomen every time one occurred. I wasn’t sure that I was in labor but I definitely knew something was going on that I needed to get checked out. I was also checking my blood pressure when I was experiencing the tightness in my abdomen and because it was spiking each time so I decided to go to the hospital. When I got to the hospital they checked my cervix and confirmed that I was starting to dilate and that I was in labor. Always get checked out if you have symptoms that you are unsure of in the third trimester!
Anesthesia to Prevent Autonomic Dysreflexia
Even though most women with spinal cord injuries can’t feel the pain associated with childbirth, it is often advised to have an epidural, especially those with injuries T6 or higher, even if having a vaginal birth. An epidural is the most effective way to control and prevent autonomic dysreflexia. Consultation with an anesthesiologist should take place early on in the pregnancy to make sure a plan is in place. If labor occurs before an epidural is available or if blood pressure remains high despite the epidural, blood pressure can be controlled with oral or intravenous medications during delivery.
My Personal Experience
In both of my pregnancies I met with anesthesiologists early in the pregnancy to talk about options to control autonomic dysreflexia. I knew that I was going to have a C-section so the options were an epidural or general anesthesia. I wanted to be awake for the surgery so I chose an epidural for my first pregnancy. I remember the experience getting the epidural as distinctly unpleasant. I was shaking and really cold and could barely concentrate on the birth of my son. And because it was a surgery, I was taken to recovery after the C-section and was not allowed to see by son or husband for an hour. Then I was taken back up to a high risk pregnancy floor and not given much support as a new mom. I didn’t learn how to breast feed and my son was bottle fed right away without my permission or knowledge. I went home not even attempting to breast feed and without any resources for new moms. My first birth experience was definitely not great.


When my daughter was born it was much better. Because I went into labor early and my regular obstetric team was not available, I was admitted to the hospital like any other patient. I was not considered high risk and I was pretty much treated like any able bodied woman. The surgeon that saw me asked if it would be ok to just do general anesthesia because he was not very familiar with doing epidurals on someone with a spinal cord injury. I agreed and had a much more pleasant experience with general anesthesia (although since then I have read that general anesthesia is risky for the baby because they receive the anesthetic along with you). I was woken up directly after my daughter was born just in time to see her before they said they had to take her to the NICU because she was struggling to breath a little bit. I was discharged after 2 nights, but my daughter had to stay in the hospital for 20 days. Normally they have special rooms for parents to stay in at the hospital but none of them were wheelchair accessible so I had to drive back and forth to the hospital every day. It was super hard for me to leave my baby at the hospital every night but the time flew by pretty quickly.

Summary
Third Trimester
- The growing baby can displace your diaphragm, reducing your lung capacity. For woman with spinal cord injuries, who already have lower lung capacity, this can make breathing more difficult.
- Weight gain and other issues can make the skin more vulnerable to breakdown late in the pregnancy. Prioritizing pressure relief should be a focus throughout the third trimester.
- Autonomic dysreflexia and preeclampsia are both conditions that can cause high blood pressure in the third trimester. The treatment for each is very different so its important to always monitor your symptoms and get them checked out if you are regularly experiencing high blood pressure.
Labour and Deliver
- A vaginal birth is the preferred option for woman with spinal cord injuries. Often a vaginal birth is easier for women with SCI because they can not feel pain and their contractions are more effective without tense muscles.
- Recognizing signs of labor can be difficult without being about to feel contractions. Watching for other signs of labor such as back pain, bladder spasms, or autonomic dysreflexia can be useful.
- Anesthesia is important for most women with SCI no matter what type of birth they are having. An epidural is the most effective way to prevent autonomic dysreflexia.
Figuring it All Out
Becoming a parent for the first time is scary for everyone. No one really knows what they are doing. Having a disability doesn’t really change that. It just means that we have a few more things to figure out than most.
It can be challenging getting everything in place that we feel we might need as a parent with a disability, but if my experiences have taught me anything, it’s that we all figure it out as we go.
And the beautiful thing is, your kids don’t have high expectations. If you give them your best and you love them, that’s enough. So don’t stress. Just have fun and watch the beauty unfold.
Before you go, don’t forget to download these free resource :
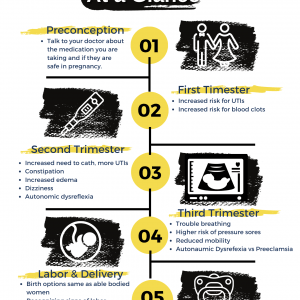
Pregnancy with a Spinal Cord Injury at a Glance
AND
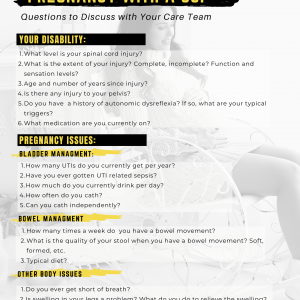
Questions to Discuss with you Care Team Before and During Pregnancy